About
Diabetes
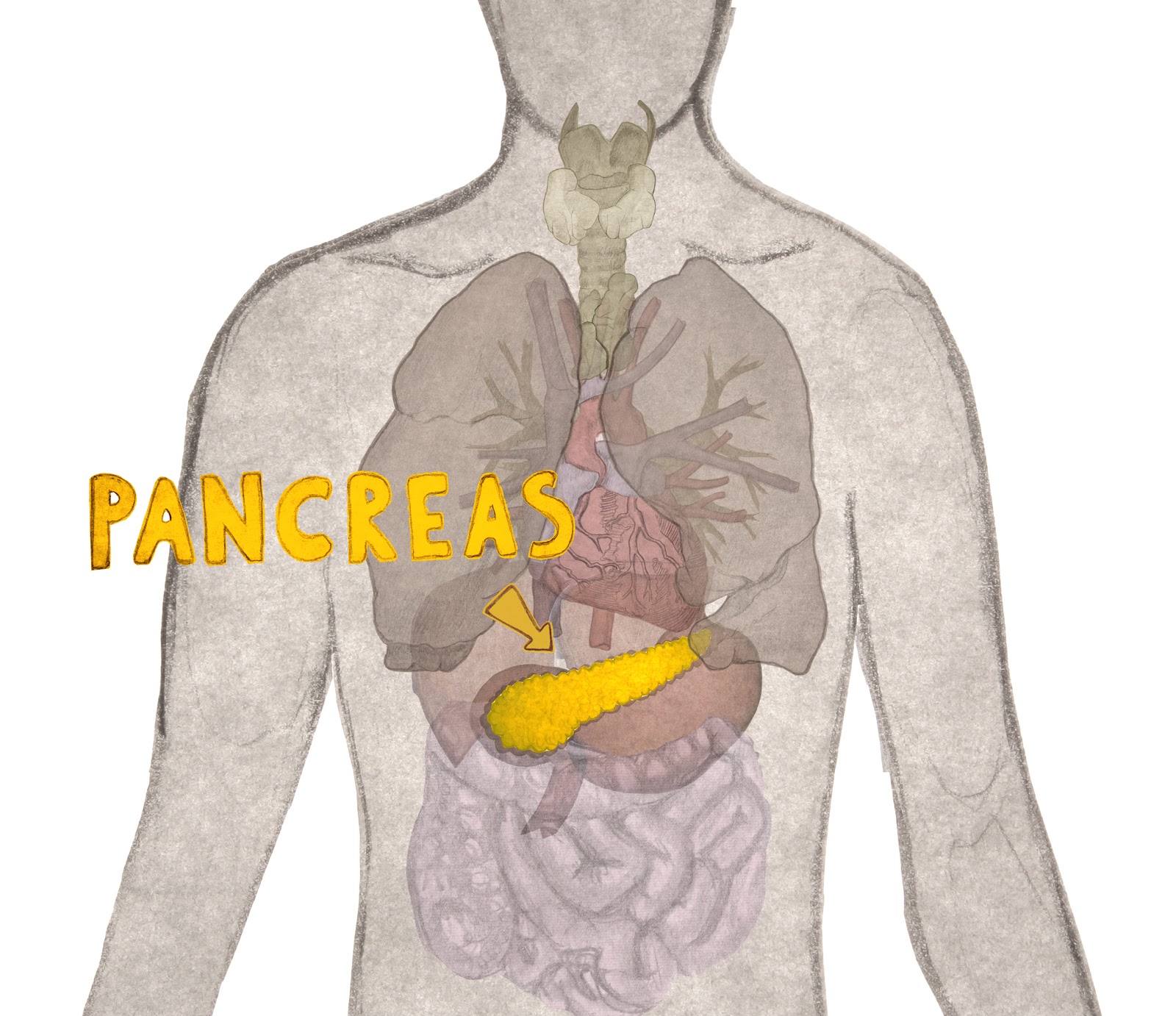
In healthy individuals, the beta cells in the pancreas release insulin in response to an increase in blood glucose levels (for example, after food intake). Insulin tells cells throughout the body to take up glucose from the blood. This is how the cells of our body gain energy from the food we eat. As diabetes affects beta cells, people living with diabetes are not able to produce insulin or use it effectively. This leads to raised glucose levels in the blood (known as hyperglycaemia). Over the long-term, high glucose levels are associated with damage to the body and leads to the failure of various organs and tissues.
Current
treatments
Treatments offered to patients with Type 1 Diabetes depends on the type and severity of the diabetic condition. Type 1 Diabetic’s make little or no insulin and so rely on daily insulin injections or an insulin pump.
With these treatments a patient must carefully and continuously monitor their blood sugar levels since the insulin delivered can never replicate the islet’s fine tuned control Improper management of insulin injections can lead to fluctuations in blood sugar levels that cause systemic damage to the individuals body. The chronic symptoms of Type 1 Diabetes affects the patients quality of life and can lead life threatening health complications.
For some extremely severe cases, a transplant is the only option. In this procedure islets – clusters of cells found within the pancreas that mainly contain insulin-producing beta cells and glucagon-producing alpha cells – are isolated from deceased organ donors. The isolated islets are then transferred to patients via the portal vein of the liver. Islets help to create a fine tuned response to fluctuations in glucose in people without diabetes. The fantastic benefit of islet transplantation is that it is the only way to completely restore normal blood sugar levels. Secondary long term complications of Type 1 Diabetes are thereby also prevented.
The challenges associated with islet transplantation include the need for more than one transplant and that donors are a very limited source of islets. Those that receive transplants also need immunosuppressive drugs to prevent transplant rejection, which in turn leaves them vulnerable to infections.
Our
innovation
We know that people with severe diabetes who have received an islet transplant experience better regulation of their blood glucose levels than can be achieved with insulin injections or pumps.
Importantly, these comparisons between current treatment approaches provide strong support that our next generation cell-therapy solution is the right treatment approach. Using stem cells as the starting point, we will develop a cell-therapy product consisting of clusters of cells reminiscent of the islets found in the pancreas. Thus, our next generation cell-therapy will create the fine-tuned benefits of an islet transplant without the challenges of using donor pancreas cells. Discover more: NEXT GENERATION CELL-THERAPY<//a>
Stories from those living with diabetes


Elena Vakali
I came across the ISLET programme really recently. I’ve been dreaming of something like this to happen since high school. When I first heard about stem cells from my father his eyes filled with hope. I think it’s something that can lead to less stress, better blood glucose control, lower chances of complications (which is a big weight over our heads all the time). I can improve our life quality and why not our life expectancy as well.
I am 29 years old and from Greece. I am a doctor, currently interning in endocrinology. My greatest interest is diabetes. I like explaining to people about diabetes and helping them with it or preventing them from developing it. I also like sports, tennis in particular, and cooking. I like finding my own recipes and trying to make the traditional Greek food healthier because there is too much fat in there.
I was around 13 years old when I was diagnosed. I was terrified. I was crying. It was really bad because while we were on our way to the hospital, before I got diagnosed, they told me that I might have diabetes and the only thing I knew about it was that my grandmother had died from diabetes. I was like, am I going to die?
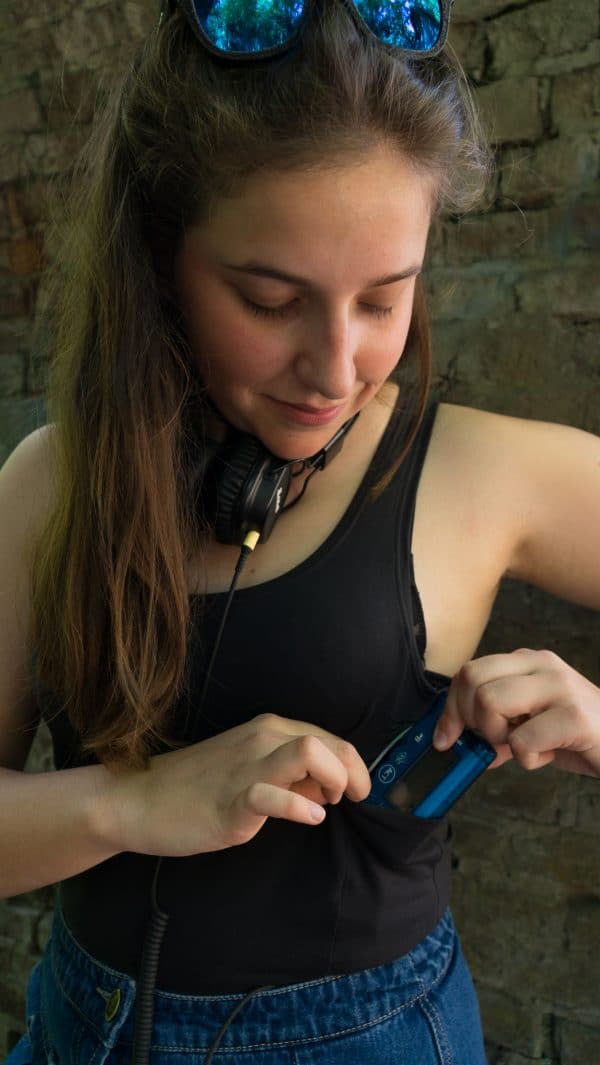
As for treatment, I have had an insulin pump for the past four years. It is really great actually, considering the fact that I didn’t want to put a pump on my body. As for my lifestyle, I am trying to eat healthily (hence the healthy cooking), exercise multiple times a week, walk and to sleep a bit. I’m trying to do everything that’s ‘doctor-recommended’.
Diabetes is more of a psychological burden. I am scared of getting complications. Every time my blood sugar goes up, I go crazy. I don’t like the fact that I have to stop doing things I want to just because my blood sugar is low or high. My wish would be to have a complications-free life, so that you don’t have to lose the things you love, or be in pain, or not be able to see the people you love. In order for that to happen, I think it’s paramount to have access to technology or medication.


Alexandra Costa
I was ten when I was diagnosed. I reacted well. I understood that it was forever, but it did not scare me. I believe that was because I was young, and I did not exactly understand what ‘forever’ means. We (my family) changed to a healthier kind of lifestyle. I started to exercise outside of school. And of course, I had to introduce the diabetes treatments. Twenty-five years ago, I had to inject three or maybe four times a day. The treatment is much better nowadays than before. I have to inject more times but it’s better for my health and my diabetes control. I have had a pump since 2010. It took me a year to believe the pump was a good treatment, because it is a thing that is outside of me. Imagine 10 years ago, if I wanted to wear skinny jeans, where do I put the pump? It was hard for me to go around and dance at night.
I am 36 years old and from Lisbon, Portugal. I have completed a bachelor’s and a master’s degree in Education and am now starting a PhD at the Education Institute of Lisbon University. I also work at APDP, the Portuguese Diabetes Association as an educator in diabetes and chronic diseases. Other than the world of diabetes, my greatest interests are sports and my family, especially my daughter.
I live in the present and try to educate society about how people with diabetes could live better in our society. I fight for better conditions for all of us. I also believe that younger people should be involved in political decisions. They should be listened to by the government and the people who make decisions about health. We are people with diabetes but mostly we are people. We are people who want to live a full life, to have work, to have a family. It would be easier if we had more help from the government doing that.




Comments and Questions
0 comments